Clinical practice guidelines often struggle to implement a mandate in the world of real medicine. For this reason, the initiatives born in the professional world that rely on instruments within reach such as persuasion, training and clinical audit are genuinely remarkable.
To illustrate what I mean, I have chosen three projects from the sensitive field of hospital infections. The first is from a team of intensive care specialists in Michigan, the second of a group of Spanish intensivists lead by Mutua de Terrassa and the third of a multidisciplinary group from Sevilla.
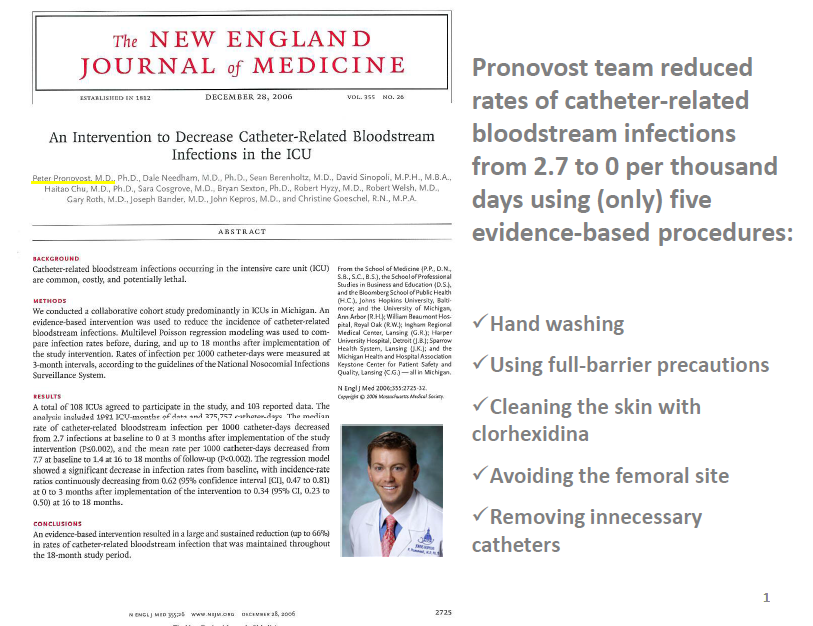
Dr. Pronovost and his team promoted a study in 108 intensive care units, where it was shown that if compliance to a very basic model is guaranteed (see above figure), catheter bacteraemia could be reduced by more than 60% and even reach rates of less than one infection per 1,000 days of catheter. Since the publication of the results of this study in 2008, most countries have rushed to deploy programs known as “bacteraemia zero."
"Edusepsis study group" headed by Dr. Ricard Ferrer in the Intensive Care Unit of the Mutua de Terrassa published the first results in JAMA of a project that was implemented in 59 Spanish intensive care units, of which I will highlight how, with a training program, it was possible to improve adherence to guidelines, and improve sepsis mortality. Later, in an article in the journal "Intensive Care Medicine" (see table above), the same group Edusepsis explained that this action protocol was cost-effective.
The third work chosen is a project lead by Dr. Cisneros (infectious disease specialist) and a multidisciplinary team of "Hospital Virgen del Rocío" in Seville. This team developed an antibiotic management program based on internal detection of inappropriate antibiotic prescriptions, and then undertook training activities aimed at the prescribing doctors through personal interviews conducted in an environment of peers. In just one year, the inappropriate antibiotic prescriptions decreased from 53% to 26% and antibiotic consumption decreased by 42%.
I wanted to title this post "professional confederacy" and that corroborates the following citation from Richard Bohmer’s article in the British Medical Journal in which he speaks of clinical leadership to address the real changes in the practice of daily work, small work. That sounds easy but is not. Getting up every morning and trying to do better than the day before is only available to the best.
Jordi Varela
Editor
Dr. Pronovost and his team promoted a study in 108 intensive care units, where it was shown that if compliance to a very basic model is guaranteed (see above figure), catheter bacteraemia could be reduced by more than 60% and even reach rates of less than one infection per 1,000 days of catheter. Since the publication of the results of this study in 2008, most countries have rushed to deploy programs known as “bacteraemia zero."
"Edusepsis study group" headed by Dr. Ricard Ferrer in the Intensive Care Unit of the Mutua de Terrassa published the first results in JAMA of a project that was implemented in 59 Spanish intensive care units, of which I will highlight how, with a training program, it was possible to improve adherence to guidelines, and improve sepsis mortality. Later, in an article in the journal "Intensive Care Medicine" (see table above), the same group Edusepsis explained that this action protocol was cost-effective.
The third work chosen is a project lead by Dr. Cisneros (infectious disease specialist) and a multidisciplinary team of "Hospital Virgen del Rocío" in Seville. This team developed an antibiotic management program based on internal detection of inappropriate antibiotic prescriptions, and then undertook training activities aimed at the prescribing doctors through personal interviews conducted in an environment of peers. In just one year, the inappropriate antibiotic prescriptions decreased from 53% to 26% and antibiotic consumption decreased by 42%.
I wanted to title this post "professional confederacy" and that corroborates the following citation from Richard Bohmer’s article in the British Medical Journal in which he speaks of clinical leadership to address the real changes in the practice of daily work, small work. That sounds easy but is not. Getting up every morning and trying to do better than the day before is only available to the best.
Jordi Varela
Editor




No comments:
Post a Comment